Leukorrhea causes, symptoms, diagnosis and treatment?
Leukorrhea causes, symptoms, diagnosis and treatment?
What is Leukorrhea
Leukorrhea is a medical term that refers to a white or yellowish vaginal discharge. It can be a normal physiological response or a sign of infection or other medical conditions, depending on the cause.
Leucorrhea is a white discharge from the vagina, which is generally normal and healthy as it helps cleanse the vagina by shedding cells and fluids, removing germs, and preventing infections. However, if the discharge changes in color, consistency, or develops an odor, it may signal an underlying issue. If you notice these changes, it’s important to consult a gynecologist for further evaluation.
Types of Leukorrhea:
- Physiological Leukorrhea:
- Occurs due to hormonal changes, particularly during ovulation, pregnancy, or sexual arousal.
- The discharge is usually clear or white, odorless, and does not cause irritation.
- Pathological Leukorrhea:
- May indicate an infection, such as a yeast infection, bacterial vaginosis, or sexually transmitted infections (STIs).
- The discharge may be thick, have an unpleasant odor, and be accompanied by itching, redness, or irritation.
-
What are the causes of likoria?
Some possible likoria causes are:
Leukorrhea, commonly referred to as “likoria” in some regions, is a condition characterized by excessive vaginal discharge. While vaginal discharge is normal and can vary throughout the menstrual cycle, excessive or abnormal discharge may indicate an underlying issue. Some common causes of leukorrhea include:
-
Hormonal Imbalance:
- Pregnancy: Increased estrogen levels during pregnancy can lead to more vaginal discharge.
- Menstrual Cycle: Variations in hormones during different phases of the menstrual cycle can cause leukorrhea, especially around ovulation.
-
Infections:
- Bacterial Vaginosis (BV): An overgrowth of harmful bacteria in the vagina can lead to a grayish or whitish discharge with a foul smell.
- Yeast Infections (Candidiasis): A fungal infection caused by Candida can lead to thick, white discharge resembling cottage cheese, accompanied by itching and irritation.
- Sexually Transmitted Infections (STIs): Certain STIs, such as gonorrhea, chlamydia, or trichomoniasis, can cause abnormal vaginal discharge that may be yellow, greenish, or foul-smelling.
-
Poor Hygiene:
- Improper or infrequent cleaning of the genital area, especially during menstruation, can result in bacterial growth, leading to leukorrhea.
-
Foreign Objects:
- Forgotten tampons, contraceptive devices, or other foreign objects in the vagina can cause irritation and infection, leading to discharge.
-
Vaginal Atrophy:
- Postmenopausal women may experience thinning of the vaginal walls due to decreased estrogen, leading to discharge, dryness, and irritation.
-
Allergic Reactions or Irritation:
- Vaginal discharge may be a response to irritants like soaps, perfumes, or chemicals in personal care products. Allergies to latex condoms or certain types of lubricants can also trigger leukorrhea.
-
Cervical Polyps or Inflammation:
- Conditions like cervical polyps or inflammation (cervicitis) may cause vaginal discharge, often with other symptoms like bleeding after intercourse.
-
Pelvic Inflammatory Disease (PID):
- An infection of the reproductive organs can lead to abnormal vaginal discharge, often accompanied by pelvic pain and fever.
-
Stress or Poor Diet:
- Stress, malnutrition, or a diet lacking in essential nutrients may impact vaginal health, sometimes resulting in leukorrhea.
In most cases, leukorrhea is not a serious condition, but when it’s accompanied by unusual odor, itching, irritation, or discomfort, it’s important to seek medical advice for diagnosis and treatment.
Common Causes:
- Hormonal fluctuations (menstruation, pregnancy, menopause)
- Infections (yeast infections, bacterial vaginosis, STIs like chlamydia or gonorrhea)
- Irritation from chemicals (douches, scented soaps, or contraceptive devices)
What are the symptoms of likoria ???
The symptoms of leukorrhea (likoria) can vary depending on the underlying cause. While some vaginal discharge is normal, certain signs may indicate an abnormal condition. Here are the common symptoms associated with leukorrhea:
- Excessive Vaginal Discharge:
- The primary symptom of leukorrhea is an increase in the amount of vaginal discharge, which may be white, yellowish, or slightly gray.
- Changes in Discharge Consistency:
- The discharge may be thick, watery, or frothy. In cases of yeast infections, it might appear thick and resemble cottage cheese.
-
Foul Odor:
- Leukorrhea due to bacterial infections like bacterial vaginosis or sexually transmitted infections (STIs) may have a fishy or unpleasant smell.
- Itching or Irritation:
- Many women experience itching, burning, or irritation in the vaginal or vulvar area, especially in cases of yeast infections or allergic reactions.
- Pain or Discomfort:
- Pain or discomfort in the pelvic region, or during urination or intercourse, can occur in cases where leukorrhea is associated with infections or conditions like pelvic inflammatory disease (PID).
-
Color Changes in Discharge:
- Discharge color may vary depending on the cause:
- White or Clear: Often seen with hormonal changes (e.g., pregnancy, ovulation).
- Yellow or Greenish: May indicate a bacterial or sexually transmitted infection.
- Grayish: Often seen in bacterial vaginosis.
- Lower Abdominal Pain:
- In some cases, leukorrhea can be accompanied by lower abdominal pain, particularly when caused by conditions like PID or other infections.
- Burning Sensation During Urination:
- If leukorrhea is caused by an infection, you may experience a burning sensation when urinating.
- Frequent Urination:
- Increased urinary frequency may accompany leukorrhea in certain cases, especially when there is an infection affecting the urinary or reproductive organs.
- Vaginal Dryness (in some cases):
- Postmenopausal women or those with vaginal atrophy may experience both excessive discharge and dryness or irritation.
If leukorrhea is accompanied by symptoms like itching, foul odor, pelvic pain, or an unusual color or consistency of the discharge, it’s essential to seek medical evaluation to rule out infections or other conditions.

What do different colors of vaginal discharge indicate?
Different Colors of Vaginal Discharge and Their Meanings
Leukorrhea or vaginal discharge, can present in various colors, each potentially indicating different conditions. Understanding what these colors signify is important for maintaining vaginal health. Here’s a guide to what each color may suggest:
- Clear:
Clear discharge, often resembling egg whites in consistency, is typically a sign of a healthy vagina expelling dead cells and bacteria. This discharge is common during ovulation, pregnancy-related hormonal changes, or sexual arousal. - Milky White:
Discharge ranging from creamy to milky white is generally normal unless accompanied by an unusual odor or texture. This is simply the vagina’s natural way of self-lubricating and cleansing. -
Yellow to Green:
While light yellow discharge may be normal, darker yellow or green discharge could indicate an infection. It’s important to consult a gynecologist for appropriate tests. If no infection is found, the discharge color may be influenced by your diet.
- Pink:
Pink discharge, whether light or deep, often occurs just before the start of a menstrual cycle or after intercourse. In some cases, however, it may indicate an underlying health issue that requires medical attention. -
Red or Brown:
Red or brown discharge is typically normal before, during, or right after menstruation. However, if it occurs at other times, it could indicate a health concern that needs to be evaluated.
- Grey:
Grey discharge is a common sign of bacterial vaginosis, especially if it is accompanied by an odor. Immediate medical consultation is recommended, and treatment typically involves topical or oral antibiotics.”**

How can likoria be diagnosed?
Leukorrhea (likoria) can be diagnosed through a combination of patient history, physical examination, and laboratory tests. If a woman experiences abnormal vaginal discharge or associated symptoms, a healthcare provider will follow several steps to determine the cause. Here’s how leukorrhea is typically diagnosed:
-
Medical History:
The doctor will begin by asking about your symptoms, including:
- The color, consistency, and odor of the discharge.
- When the symptoms started and how long they have lasted.
- Presence of other symptoms like itching, burning, pain during intercourse, or lower abdominal pain.
- Menstrual history, sexual activity, contraception use, and any recent infections or antibiotic use.
-
Physical Examination:
A pelvic examination is often performed to visually assess the vaginal and cervical areas for signs of infection, inflammation, or lesions. The doctor will:
- Inspect the vagina and cervix for redness, swelling, or discharge.
- Check for any signs of vaginal or vulvar irritation.
- Conduct a bimanual exam to evaluate any tenderness or abnormal growths in the pelvic area.
-
Lab Tests and Diagnostic Procedures:
- Vaginal Swab: The doctor will often take a sample of the vaginal discharge using a swab. This sample is then examined under a microscope or sent to a lab for analysis to check for:
- Bacterial infections like bacterial vaginosis (BV).
- Fungal infections like candidiasis (yeast infection).
- Sexually transmitted infections (STIs) such as gonorrhea, chlamydia, or trichomoniasis.
- pH Testing:
The vaginal pH level can also be measured using a litmus paper. A higher than normal vaginal pH can indicate bacterial vaginosis or a trichomoniasis infection. -
Culture Test:
Sometimes, the vaginal discharge is cultured to grow and identify specific bacteria, fungi, or pathogens causing the infection. This is useful if the exact infection isn’t immediately apparent.
- Pap Smear:
A Pap smear may be done to check for abnormal cervical cells or conditions such as cervicitis (inflammation of the cervix), which may be contributing to leukorrhea.
-
Additional Testing:
If the cause of leukorrhea is unclear after initial tests, or if more serious conditions are suspected, further diagnostic procedures may include:
- Ultrasound: To check for pelvic inflammatory disease (PID) or abnormalities in the reproductive organs like polyps or fibroids.
- Blood Tests: To detect systemic infections or sexually transmitted infections that may be causing abnormal discharge.
-
STD Screening:
If the doctor suspects that a sexually transmitted disease may be the cause of leukorrhea, specific tests for STDs such as gonorrhea, chlamydia, or HIV may be performed.
By combining the information gathered from the medical history, physical examination, and lab tests, the healthcare provider can diagnose the underlying cause of leukorrhea and recommend appropriate treatment.
Treatment of leukorrhea
How can likoria be treated?
The treatment for leukorrhea (likoria) depends on its underlying cause. If the condition is due to an infection or other health issue, addressing that primary cause is key to resolving the symptoms. Here are the common treatment approaches for leukorrhea:
-
Bacterial Infections:
- Bacterial Vaginosis (BV):
- BV is often treated with antibiotics, either oral (e.g., metronidazole) or topical (e.g., metronidazole gel or clindamycin cream). It’s important to complete the full course of antibiotics to ensure the infection is cleared.
- Sexually Transmitted Infections (STIs):
- If leukorrhea is caused by an STI like gonorrhea, chlamydia, or trichomoniasis, antibiotics such as azithromycin, doxycycline, or ceftriaxone are prescribed. Sexual partners should also be treated to prevent reinfection.
-
Fungal Infections (Yeast Infections):
- Candidiasis (Yeast Infection):
- Antifungal treatments such as fluconazole (oral) or topical creams (e.g., clotrimazole, miconazole) are used to treat yeast infections. These medications usually relieve symptoms like thick, white discharge and itching within a few days.
- Hormonal Imbalance:
- Hormone Therapy:
- If leukorrhea is related to hormonal imbalances (e.g., during pregnancy, menopause, or menstruation), treatment may involve hormone therapy to regulate estrogen levels. In some cases, symptoms resolve naturally after hormonal fluctuations stabilize.
-
Pelvic Inflammatory Disease (PID):
- If leukorrhea is due to PID, which is a serious infection of the reproductive organs, a combination of antibiotics is usually prescribed. In severe cases, hospitalization or surgery may be necessary.
- Cervical Inflammation or Polyps:
- Cervicitis (Cervical Inflammation):
- Antibiotics or antiviral medications may be needed if the inflammation is caused by an infection. If cervical polyps are present and causing leukorrhea, they can be surgically removed.
-
Improving Personal Hygiene:
- Hygiene Practices:
- Sometimes leukorrhea can be managed by improving personal hygiene, such as:
- Washing the genital area with mild soap and water.
- Wearing cotton underwear to allow air circulation.
- Avoiding scented soaps, douches, or feminine hygiene sprays that can irritate the vaginal area.
- Changing sanitary pads or tampons frequently during menstruation.
- Sometimes leukorrhea can be managed by improving personal hygiene, such as:
-
Probiotic Treatment:
- Probiotics:
- In cases of recurrent bacterial or yeast infections, probiotics (either in supplement form or through dietary intake like yogurt) can help restore healthy vaginal flora and prevent infections.
- Dietary and Lifestyle Changes:
- Balanced Diet:
- Eating a well-balanced diet rich in vitamins and minerals, particularly those supporting immune health (like Vitamin C and zinc), may help prevent infections.
- Hydration: Staying well-hydrated helps the body maintain optimal vaginal health.
- Stress Management: Reducing stress can balance hormones and potentially reduce the occurrence of leukorrhea.
-
Treatment for Allergic Reactions:
- If leukorrhea is caused by irritation from personal care products, latex condoms, or other substances, the best treatment is to eliminate the irritant and switch to hypoallergenic products.
- Natural Remedies (Complementary Treatments):
- Some people use herbal remedies like fenugreek seeds, neem, or amla (Indian gooseberry) as natural treatments for leukorrhea. While these may help manage symptoms, it’s important to consult a healthcare professional before starting any alternative treatments.
- Surgical Intervention (if necessary):
- In rare cases, if leukorrhea is caused by structural abnormalities, polyps, or tumors, surgical intervention may be required to remove the cause of the abnormal discharge.
- Preventive Measures:
- Avoid unprotected sexual contact to reduce the risk of STIs.
- Maintain good genital hygiene.
- Avoid douching, as it can disrupt the natural balance of bacteria in the vagina.
If you experience unusual or persistent leukorrhea, it’s important to seek medical advice to determine the cause and appropriate treatment. Proper diagnosis is crucial for effective treatment and to prevent complications.
Now I am giving leukorrhea treatment with using medicine. Leukorrhea may cause different reason so treatment is required with different angle here I am giving the treatment only using medication according to condition. Some direct prescription are given bellow you may use anyone according to your present physical condition.
It is important to know when you would use medicine or this prescription to prevent leucorrhea.
When to Seek Medical Attention:
- Changes in the color, consistency, or smell of the discharge.
- Accompanied by itching, burning, or pain during urination or intercourse.
- Persistent or unusual discharge that does not resolve on its own.
If you’re concerned about leukorrhea, it’s important to consult a healthcare professional for an accurate diagnosis and treatment.
When you don’t need any medicine or any treatment:
- Clear discharge and smell less
- When vaginal discharge is milky in color
- White in color, Slightly sticky nature
- Leukorrhea occurred by hormonal change during pregnancy or prior to started menstrual cycle
Above this condition you don’t need use any medicine; it is natural process of human body. If vaginal heavy discharge occurred with color and consistency frequently you may need for some hormonal balancing treatment.
When you need medicine or any treatment:
- Color discharge and odor smell
- When vaginal discharge is yellow to green in color
- Grey color of vaginal discharge
- The discharge may be thick, watery, or frothy. In cases of yeast infections, it might appear thick and resemble cottage cheese.
- Foul odor
- You may experience itching, burning, or irritation in the vaginal or vulvar area, especially in cases of yeast infections or allergic reactions
- May feel pain or discomfort in the pelvic region, or during urination or intercourse
During vaginal discharge with above symptoms you should need medication as treatment. Two prescription are given bellow-
Prescription no 1
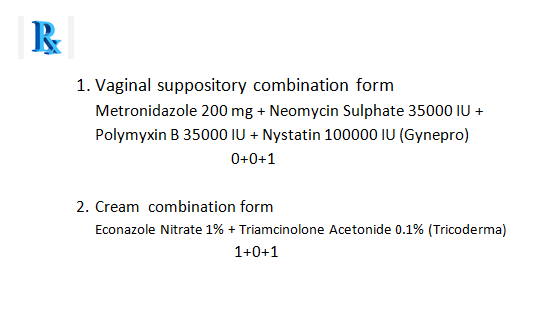
Vaginal suppository should insert into vagina at every night before go to bed and cream should use two times a day in to vaginal surface area.
The prescription no 1 should be used minimum for 7 days if leucorrhea doesn’t cure medicine should continue for more 7 days.
who can’t use prescription no 1:
- Basically don’t fount any contraindication the medicine of prescription no 1 , some specific medicine can shown hyper sensitivity and may shown little side effect although not significant result that you prohibited this prescription for using.
- Pregnant or lactation patient should not use this prescription.
If prescription no 1 doesn’t work well you may use prescription no 2:
Prescription no 2
It should be allow for all above 14 years old patients.
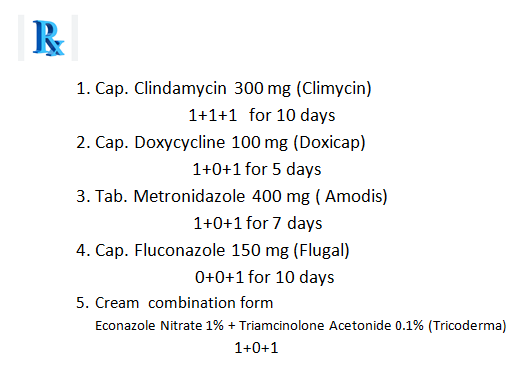
Cream should use two times a day in to vaginal surface area.
who can’t use prescription no 1:
- Hyper sensitivity for specific medicine
- Pregnant or lactation patient should not use this prescription.
- Severe liver cirrhosis patient
- Severe kidney disease patient.
What do you feel changes or side effects by using prescription no 2:
- Abdominal pain
- Oesophagitis and oesophagial ulcer
- Nausea
- Vomiting and diarrhea
- Pruritus
- Skin rashes
- Urticaria
- Fatulence
If you’re concerned about leukorrhea, it’s important to consult a healthcare professional for an accurate diagnosis and treatment.
If anyone want to more information please send to me your question through the given email address.
Email address: mallicktarun@rocketmail.com
For getting treatment base suggestion please contact or request an appointment.
