Osteoarthritis symptoms and treatment.
Osteoarthritis symptoms and treatment ??
What is Osteoarthritis ??
Osteoarthritis (OA) is the most common form of arthritis, characterized by the degeneration of joint cartilage and the underlying bone. It primarily affects older adults but can occur at any age due to joint injury or other factors. OA typically affects the knees, hips, hands, and spine, leading to symptoms such as pain, stiffness, swelling, and reduced range of motion. Osteoarthritis (OA) is is a common chronic condition of articular designeration. Secondary changes can occur in bone leading to pain, Decreased functioning and even disability. 55 Yaar elderly people are mostly affected by osteoarthritis disease. Early age from 35 years old and less than 35 also seen affected by this disease. Women are more than three times greater affected by this osteoarthritis than man.

Pathophysiology
-By developing this disease with age the strength of tendons ligaments and muscles declines.
-By apoptosis and inhibiting Proliferation rate number of chondrocytes decline
-Decrease proteoglycans
-Increase interleukin 1 that decrease matrix metalloproteins (MMPs) Proteoglycans
– pain from ( Osteoplytes, synovitis , bursitis ,Tendonitis)
Causes and Risk Factors
- Aging: The risk increases with age due to the cumulative wear and tear on joints.
- Joint Injury: Previous injuries, such as fractures or ligament tears, can increase the likelihood of OA in the affected joint.
- Obesity: Excess body weight places additional stress on weight-bearing joints, particularly the knees.
- Genetics: Family history can influence the risk, suggesting a genetic predisposition.
- Repetitive Stress: Jobs or activities that require repetitive motion can contribute to joint wear and tear.
- Female muscle weakness,
- Obesity,
- Joint trauma,
- Heredity
- Congenital or anatomical defects
Clinical presentation
– Deep localized pain in a joint
-Crackling noise heard in the joined upon moving
-Osteoarthritis most commonly affects hips, knees, spine, feet and hands.
Symptoms
- Pain: Often worsened with activity and relieved by rest.
- Stiffness: Particularly noticeable in the morning or after periods of inactivity.
- Swelling: Caused by the inflammation of the soft tissues around the joint.
- Decreased Flexibility: A reduced range of motion in the affected joint.
- Grating Sensation: A feeling or sound of bone rubbing on bone.
Diagnosis
Diagnosis is typically made through a combination of:
- Medical History: Patient symptoms and family history.
- Physical Examination: Assessing joint tenderness, swelling, and range of motion.
- Imaging: X-rays or MRI scans can reveal joint damage, cartilage loss, and bone changes.
- Lab Tests: Blood tests may rule out other forms of arthritis.
should need proper diagnosis
- physical examination
Misshaped join, decrease range of joint motion, joint tenderness
- Laboratory test
for osteoarthritis has no specific laboratory test allow
- Reveal Synovial fluid
- Increase Leukocytosis and mononuclear lymphocytes
- Radiography
– cartilage damage resulting narrowing of joint space
– osteophyte and subchondral sclerosis are seen

Treatment
While there is no cure for osteoarthritis, treatment focuses on managing symptoms and improving quality of life:
- Medications: Pain relievers (acetaminophen, NSAIDs), topical treatments, and in some cases, corticosteroid injections.
- Physical Therapy: Exercises to strengthen muscles around the joint, improve flexibility, and reduce pain.
- Lifestyle Changes: Weight management, low-impact exercise, and a healthy diet can alleviate symptoms.
- Surgical Options: In severe cases, joint replacement or other surgical interventions may be considered.
- Assistive Devices: Braces, shoe inserts, or canes can help reduce stress on joints.
Basic treatment pattern
Treatment goal
– First goal to control pain
-Improve joint mobility
-Minimize functional disability
For osteoarthritis treatment-
Pharmacological and Non-pharmacological both treatment are simultaneously important
Non pharmacological treatment
Non pharmacological treatment are most important for the osteoarthritis patient
It may does by
-Patient education ( tips on joint protection and exercise program)
-Weight loss
– Aerobic exercise program to increase muscle strength
– Physical therapy
– Use assistive device
– Acupuncture may reduce the pain
– Thermal therapy
Pharmacological treatment
Pharmacological treatment can divided by two groups ( Mild & Acute osteoarthritis )-
1. For mild pain when initiate osteoarthritis
Medication 1
1.1 . Paracetamol
Dose : 500 mg for 4 times a day not more than 4 g a day
Or
1.2 .1. Non steroidal anti inflammatory drugs (NSAID)
Example of this medicine
1.2.1.1. Ibuprofen
Dose: 400 mg 3 times a day not more than 3200 mg per day After meal
Or
- 2.1.2. Diclofenac
It is most effective medicine for NSAIDs group
Dose: 75 mg twice a day not more than 200 mg per day should be taken after meal.
Note: People are mostly hyper gastritis symptoms or peptic ulcer disease or duodenal Ulcer disease or acute renal disease should not use this type of drug in oral form.
This type of medicine inhibit platelet activation resulted inhibit coagulation process. Ulcer patient, haemophilia or any other coagulation disorder patients should not take this medicine.
-
Other analgesic
2.1. Tramadol
Dose: 50 mg 4 to 6 hours interval for 15 days
2.2. Pregabalin
Dose: 25 mg 1 or 2 times a day Initial dose for three to five days Then increase the dose according to tolerance.
2.3. Steroid Anti Inflammatory drugs
Prednisolone
Dose: 5mg 2 times daily for 15 days.
Note : For severe diabetic patients it would be concerned about the use of this medicine. It may increase the blood glucose level.
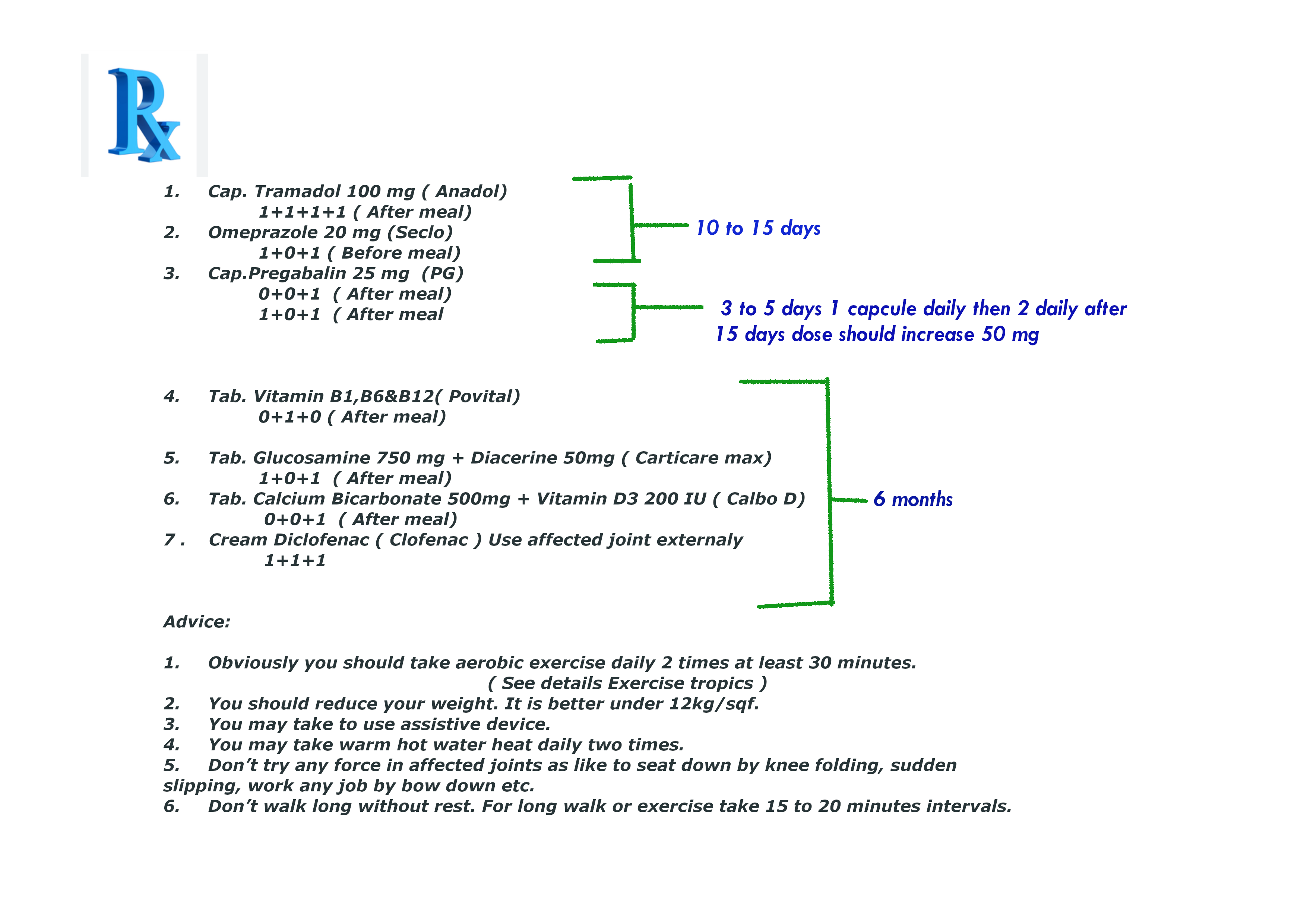
Here I am giving some direct prescription that you may use according to your physical condition. In theses prescription i use most cheap and effective medicine around the world.
Prescription –
You can follow some prescription according to your physical condition. All prescription are for adult patient who are more than 16 years old or above.
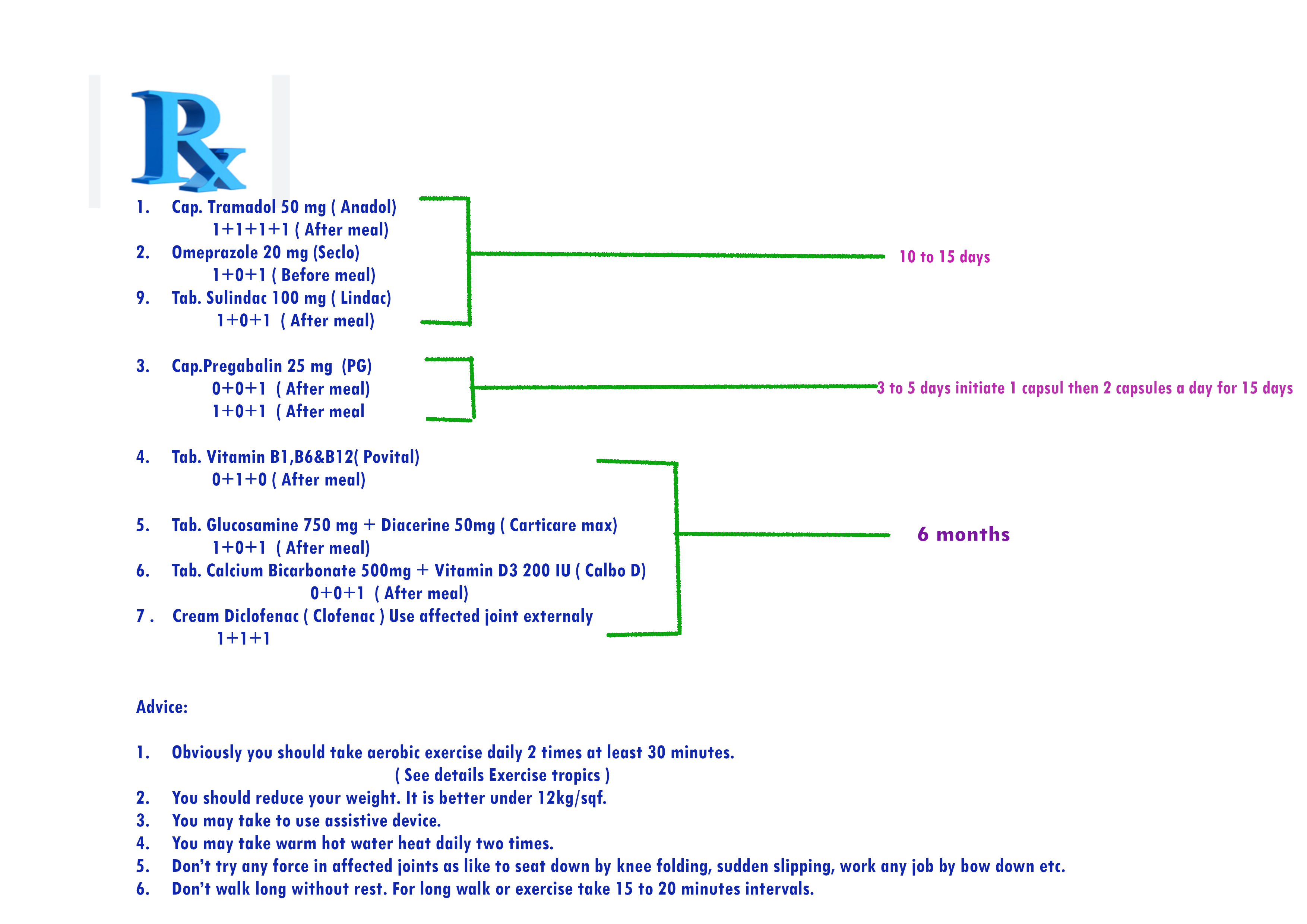
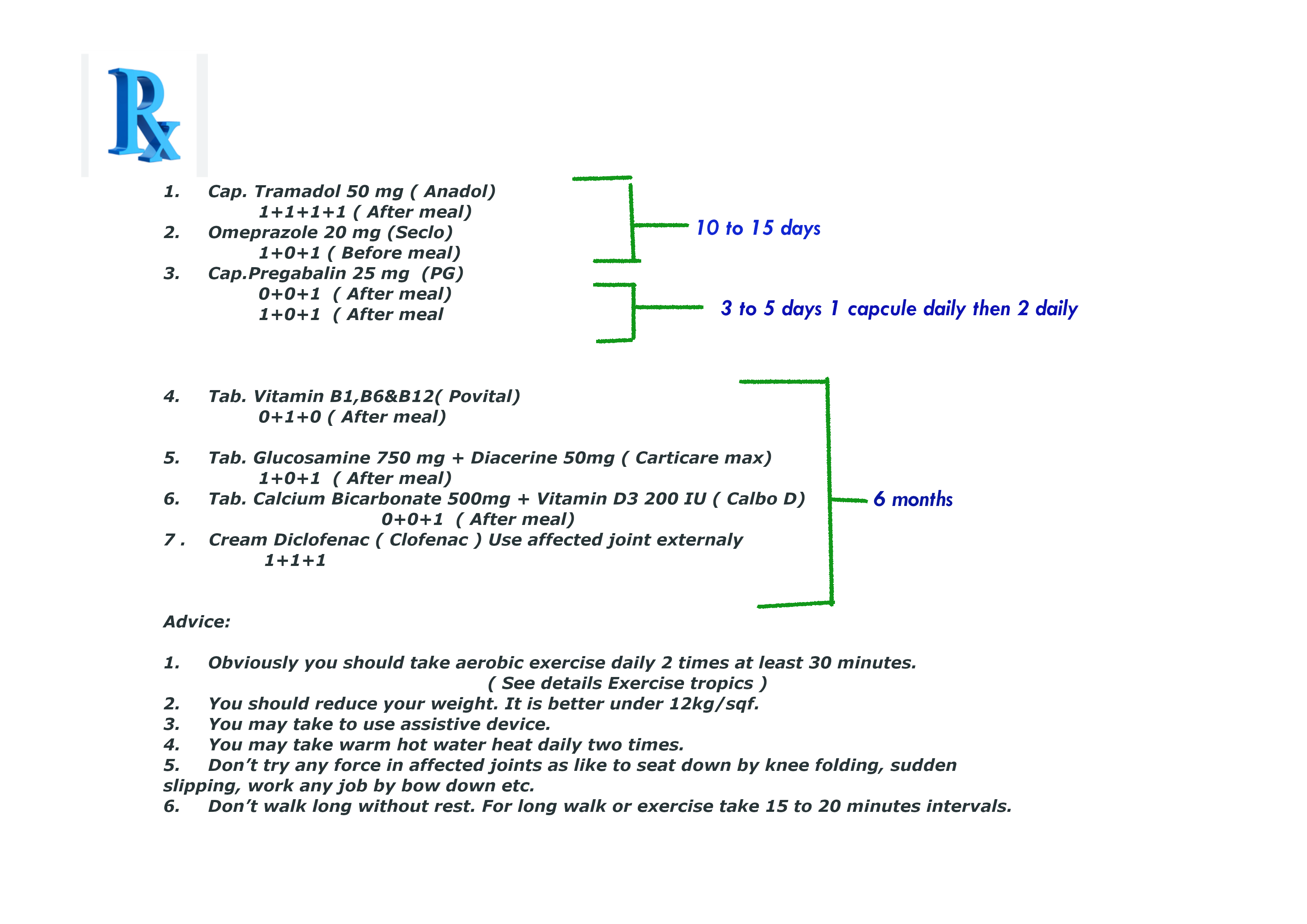
at first the prescription N0 1 & 2. for mild osteoarthritis :
Who don’t follow the prescription No. 1,2 & 3 ( Contraindication )-
Patient are suffering by post morbidity or mortality disease like
- Chronic diabetics
- Chronic kidney disease
- Chronic liver cirrhosis
- Peptic or Gastric ulcer patient and any other coagulation disorder patients like hemophilia.
- Heart failure patient
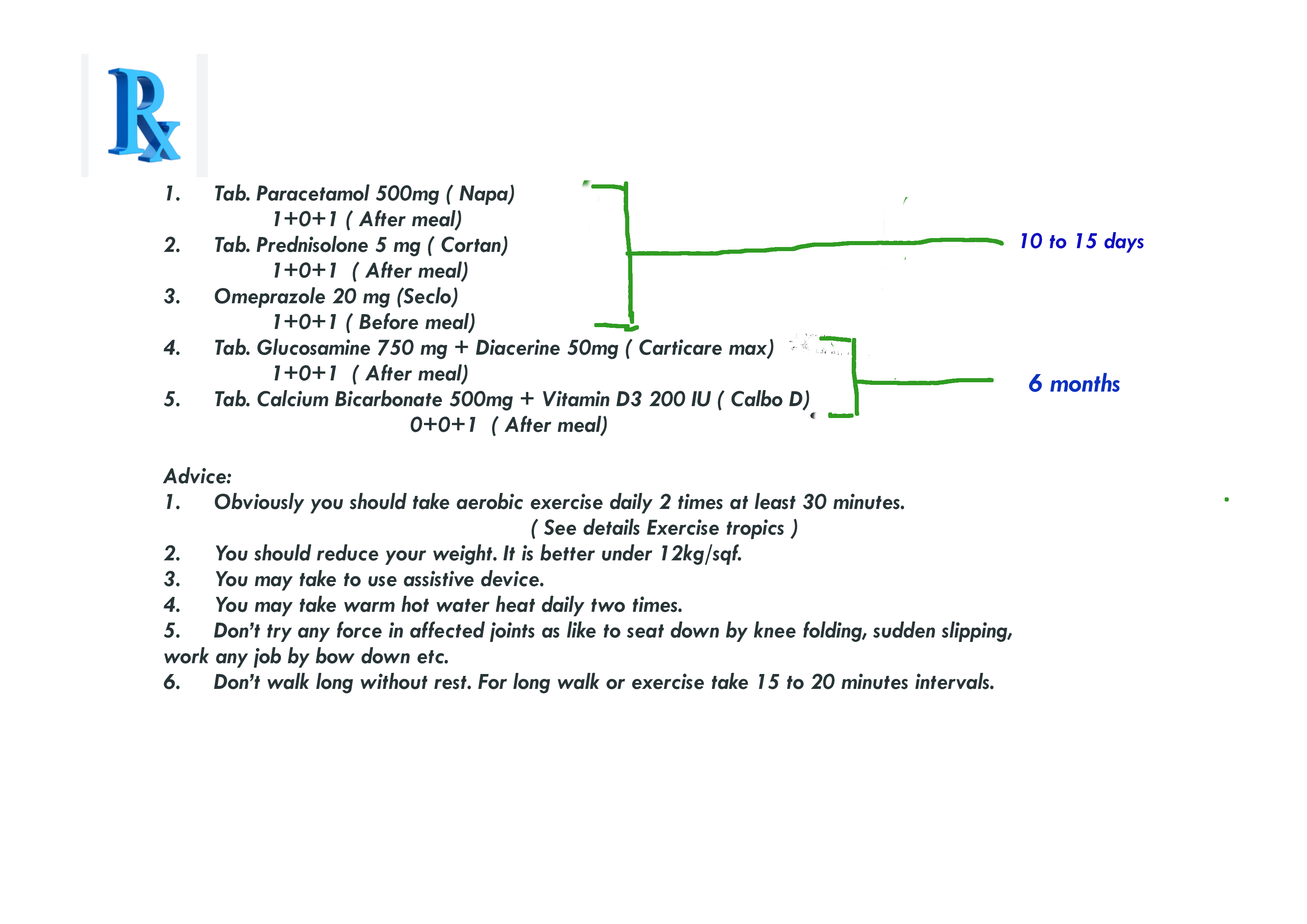
here prescription N0 1 for mild osteoarthritis patient.
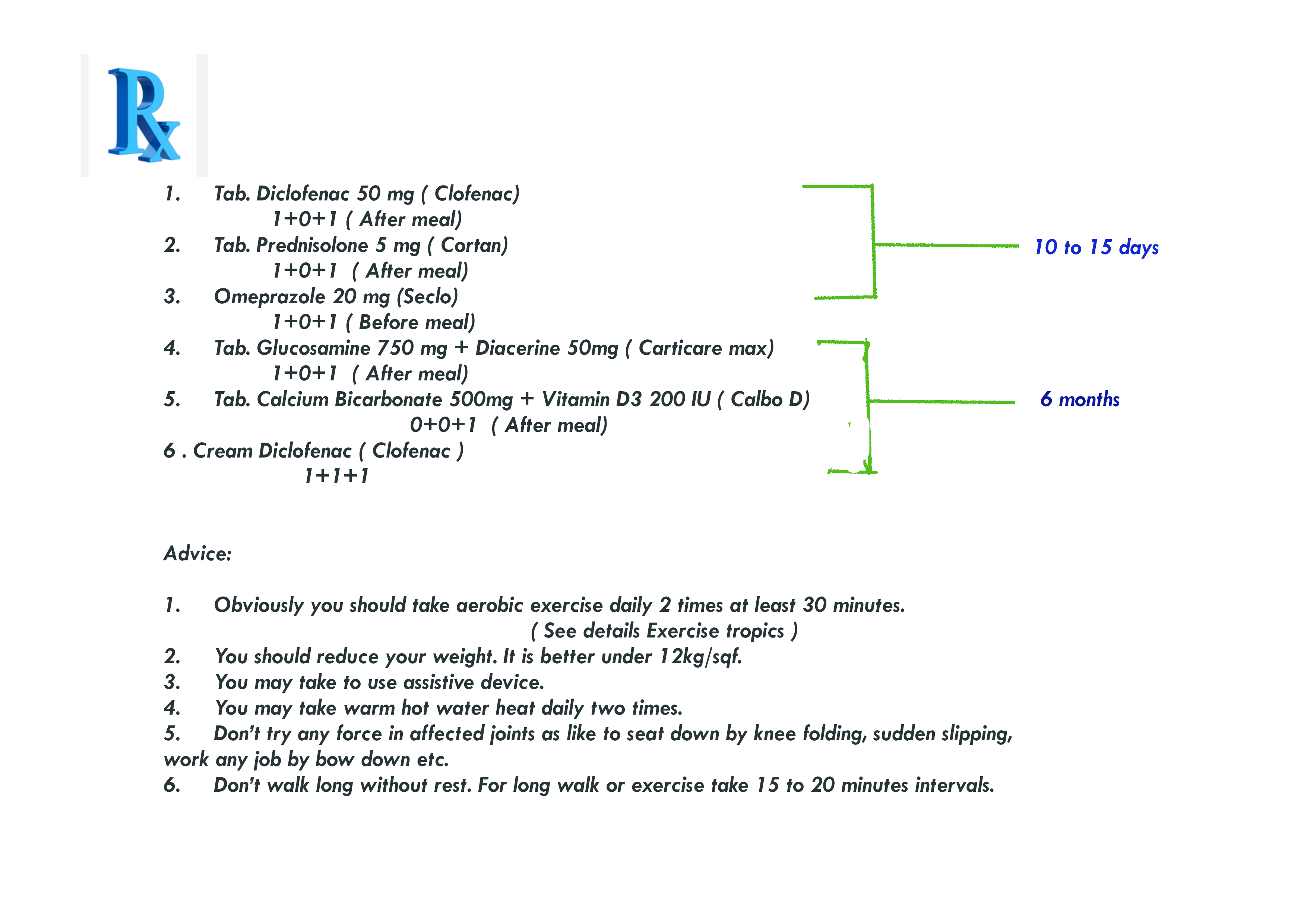
Or prescription N0 2. :
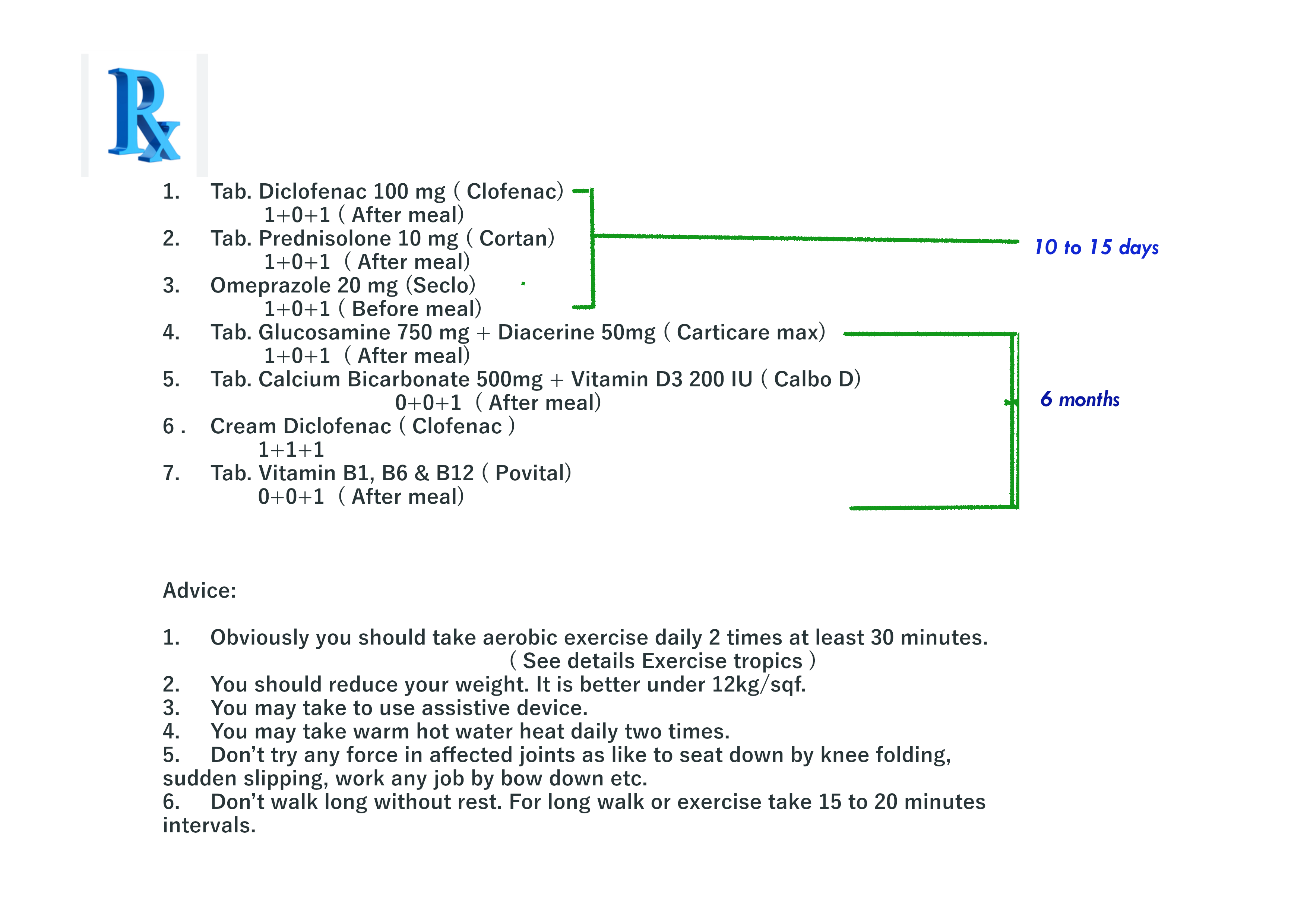
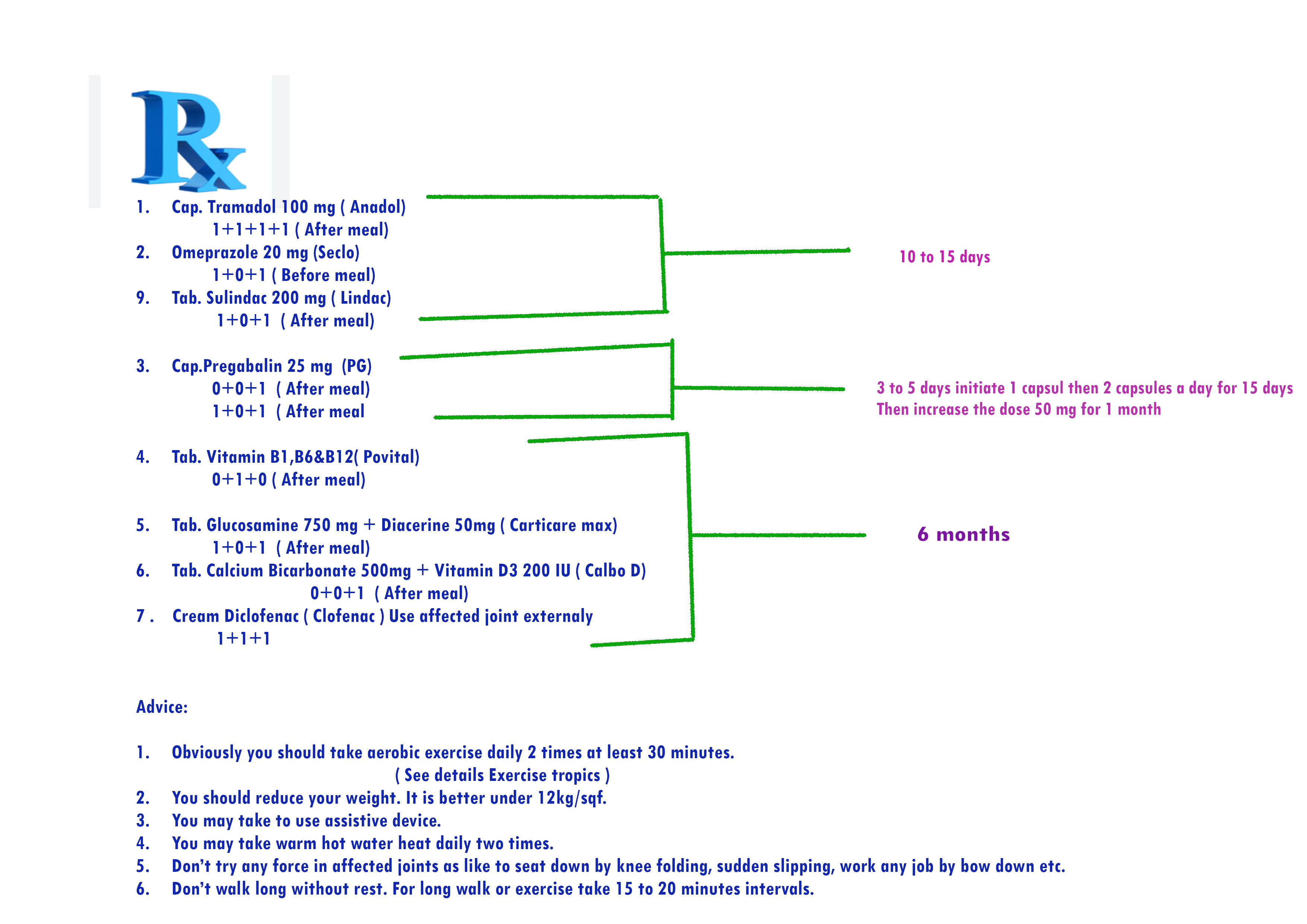
Here prescription N0 3. for acute osteoarthritis :
The prescription for osteoarthritis patient who have specific co- morbidity or mortality disease is given bellow.
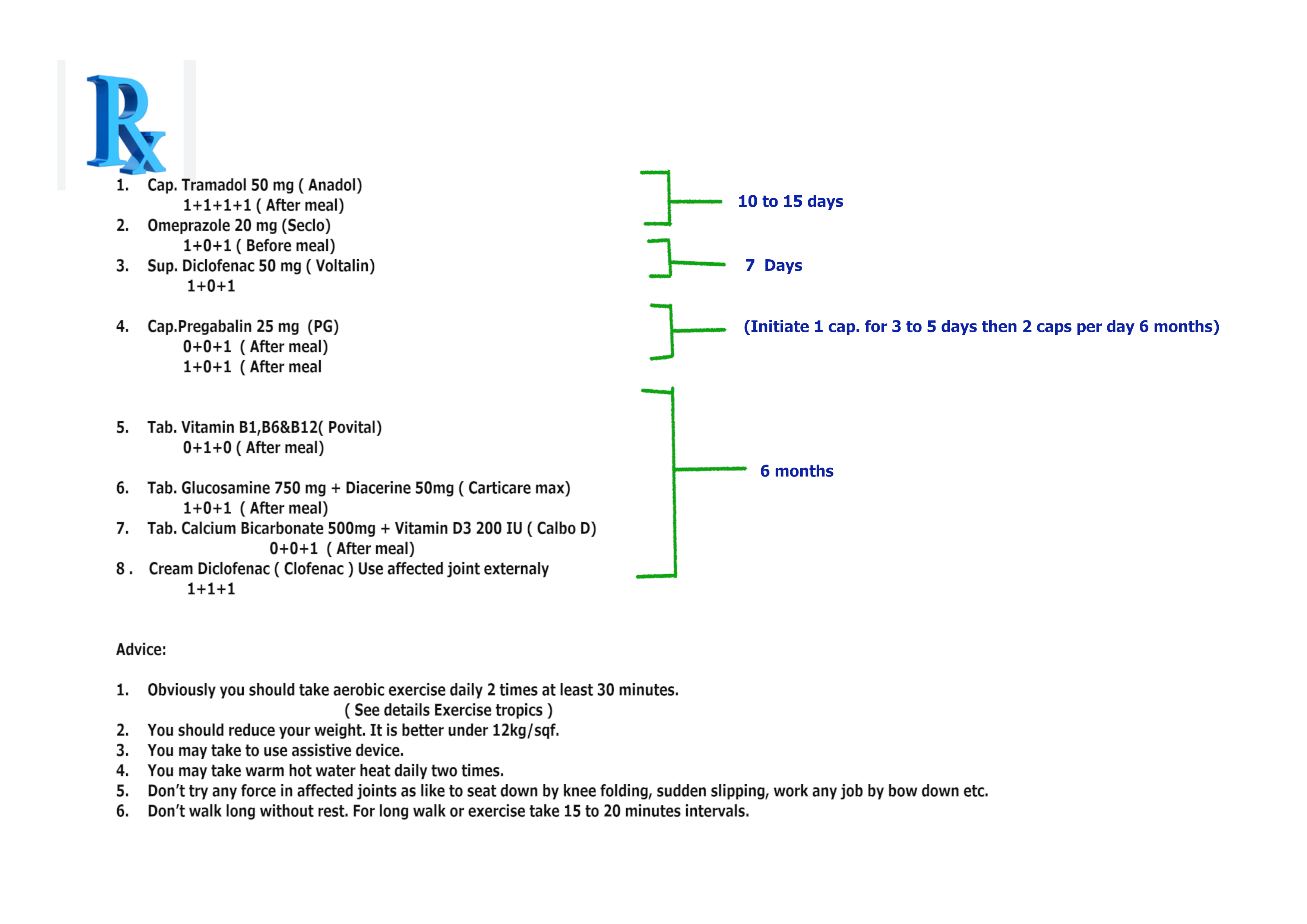
- Prescription No 4. for acute osteoarthritis patient who also a peptic or gastric ulcer patient
Who don’t follow the prescription No. 4 ( Contraindication )-
Patient are suffering by post morbidity or mortality disease like
- Chronic kidney disease
- Any other coagulation disorder patients like hemophilia.
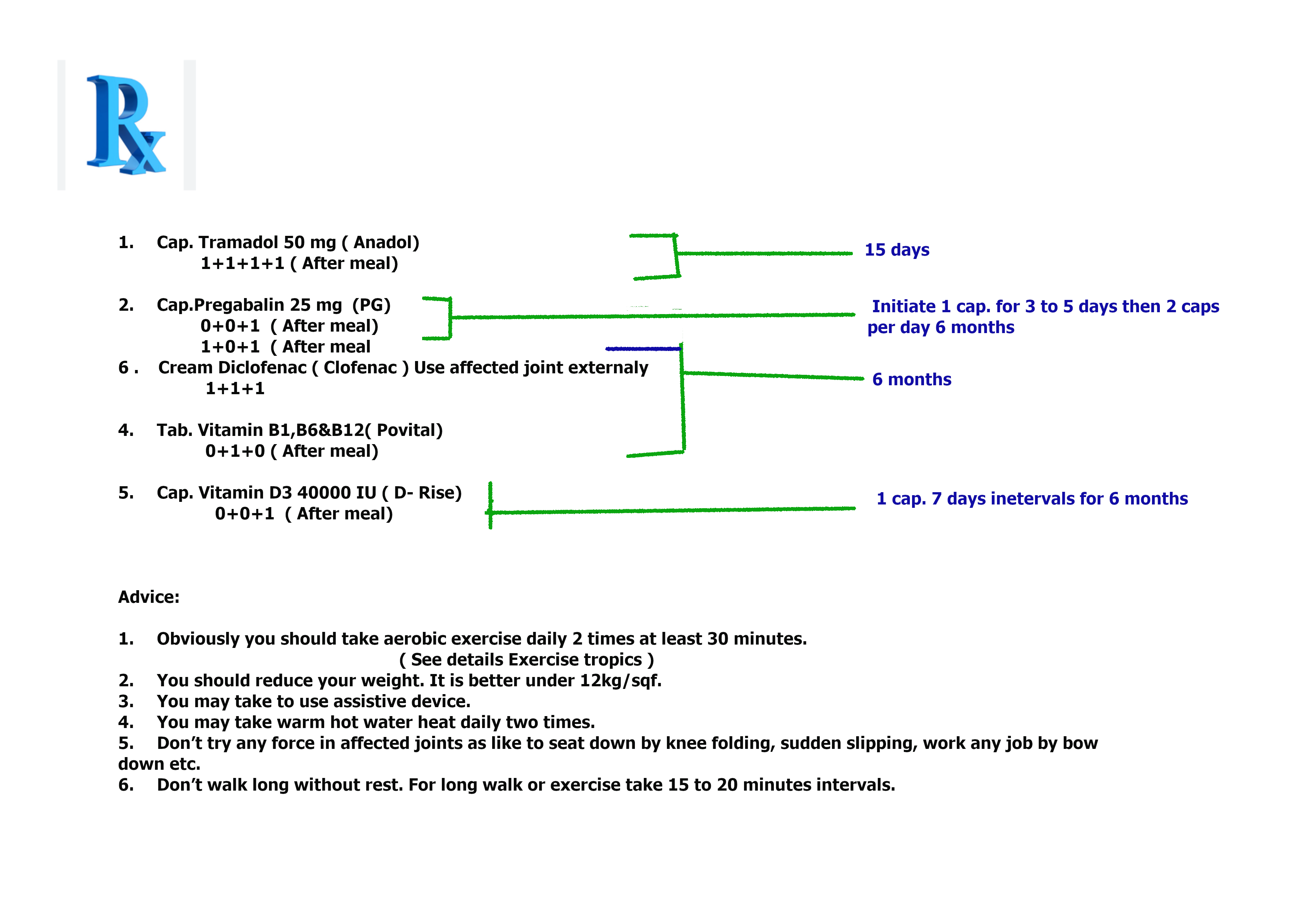
- Prescription No. 5 for mild osteoarthritis patient who have also a mild kidney disease-
- Prescription No.6 for Acute osteoarthritis patient who have mild kidney disease
- Prescription No.7 for mild and acute osteoarthritis patient who have acute kidney disease
- Prescription No.8 for mild osteoarthritis patient who have peptic or gastric ulcer and blood coagulation disorder
- Prescription No.9 for acute osteoarthritis patient who have peptic or gastric ulcer and blood coagulation disorder
Note : Prescription No 4, 5,6,7,8 & 9 is not contraindicated for diabetics patient but little conscious for liver cirrhosis patients.
-
Disease modifying anti-rheumatic drugs ( DMARDs)
It is a first line therapy for osteoarthritis and rheumatoid arthritis disease. Long time therapy more than eight months for getting effective results and withdrawal of the medicine. This therapy needs highly monitoring about the result of drug effects.
I suggest avoiding this medication for its lots of side effects and critical monitoring effects. If any patient is under a physician with strict monitoring only that patient can take these medicines.
It needs a combination therapy with two DMARDs or other DMARDs with anotherNSAIDs.
3.1. (DMARDs with others DMARDs)
[ 8 months to 2 years ]
3.1.1 Methotrexate
Dose : 7.5 to 25 mg once weekly .
With
3.1.2.. Sulfasalazine
Dose : 500 mg to 3g daily.
Side effects
Most side effects are
- GI disturbance
- Myelosuppression
- Hepatotoxicity
- Pneumonitis
- Infections.
-
Biological therapies
These drugs are used after failing DMARDs drugs. Chief class of drugs target TNF- Alpha, interleukins-1, interleukin-6 that are cytokinins mediated activate T- cell release.
4.1. Infliximab
Dose: 3 mg/kg at weeks for 0,2 and 6 weeks then 8 weeks thereafter.
Administration rout : Intravenous (IV).
OR
4.2. Adalimumab
Dose: 40 mg every two weeks
Side effects
– Lymphoma
– Infection any organ
– Immunosuppressed
– Heart failure
Note : I suggested that the Disease modifying anti-rheumatic drugs ( DMARDs) and Biological therapies if you want to take you should need close monitoring with a specialist otherwise you may avoid these medication.
Prevention
- Maintain a Healthy Weight: Reduces stress on joints, particularly weight-bearing ones.
- Exercise Regularly: Low-impact activities like swimming or cycling help maintain joint function and muscle strength.
- Avoid Joint Injuries: Protecting joints during physical activities can lower the risk of OA.
- Healthy Diet: A balanced diet rich in vitamins and minerals, especially calcium and vitamin D, supports bone health.
Osteoarthritis can significantly impact daily life, but with proper management and lifestyle adjustments, many people can maintain a good quality of life.
Note: If you suffer sever osteoarthritis attack and don’t control at home you should go hospital immediately.
If anyone want to more information please send to me your question through the given email address.
Email address: mallicktarun@rocketmail.com
For getting treatment base suggestion please contact or request an appointment.
You may also visit you tube video channel that may helpful to you.
